WP2- Virtual Populations
Population and morphology models
Watch this video (April 2022) by Noor Samuels for the latest info on the virtual population model, or this video by Nikki Boodt and Nerea Arrarta about the clot atlas, or this video by Praneeta Konduri on the vessel atlas.
In this WP, we focus on the following objectives (scroll down for updates!)
1. Development of a population model for the generation of virtual populations of stroke patients
Based on available clinical and imaging data we will develop a population model. This model consists of a set of probability density distributions of relevant parameters, including known correlations, obtained from real patient data. A virtual patient is a sample from this model and is interpolated from these distributions. As virtual patients need to be accurate representations of characteristics present in real populations of stroke patients, we include imaging derived information on vascular anatomy and thrombus, besides relevant clinical data. Furthermore, the variety and correlation of all included parameters will be taken into account as part of the population model.
2. Development of vessel segmentations, atlases of clots and ischemic cores
We will create extensive vessel models based on segmented arteries obtained from available imaging data. Also, frequency distributions and correlation matrices of different thrombus imaging characteristics, such as size (volume, length), location, distance from internal carotid artery terminus, attenuation, and perviousness will be generated. Furthermore, probability maps of thrombus locations, indicating the chance that a thrombus is present in a specific part of the intracranial arteries, will be created. In addition, we will predict the final infarct volume based on the thrombus location, thrombus composition and collateral score. Probability maps of infarcts that indicate the chance of having an infarct in a specific region based on prior clinical and imaging information will be created.
3. Correlation between clinical and imaging characteristics and clot composition
Thrombi obtained during mechanical thrombectomy will be collected and analyzed using routine macroscopy, histology and immuno-histochemistry. Clot composition will be studied by quantitative determination of the amount of red blood cells, white blood cells, platelets, fibrin and von Willebrand factor. In addition, the stent thrombus interaction as a function of the thrombus composition will be assessed by electron microscopy of the stents. The thrombus database will be used to create a clot population model. We will build statistical models to correlate histologic clot composition with (clinical and) imaging features. These models will be used to connect the in silico models of thrombolysis and thrombectomy within the virtual stroke population.
4. Correlation between procedural outcome (revascularization, reperfusion) and clinical outcome
We will develop statistical models that correlate vessel geometry and clot composition to imaging outcome parameters: revascularization, reperfusion and final infarct volume. The results of the in silico models will be compared with the results of the statistical models, allowing a validation of the in silico models on the population level. Finally, we will also relate the output of the in silico models to clinical outcome. Therefore, we will develop statistical models to predict clinical outcome (modified Rankin scale and National Institutes of Health Stroke Scale) based on available data on recanalization, reperfusion, in situ propagation of thrombus, final infarct volume, and ischemic core location.
Below an update per September 2020
The aim of WP2 was to develop and validate a population model based on available clinical and imaging data. This model should consist of a set of probability density distributions of relevant parameters, including known correlations, obtained from real patient data. Populations of virtual stroke patients can be selected to undergo virtual stroke treatments followed by outcome assessment. The virtual population model consists of a statistical module that has been fitted based on large database of real stroke patients and will be validated based on another dataset.
Virtual stroke patients are then a sample of this model and need to be realistic representatives of real stroke patients incorporating important prognostic clinical and imaging characteristics such as age, sex, cardiovascular comorbidities, collateral status and location of the intracranial arterial occlusion. The first version of the population model included 12 clinical and imaging characteristics. The discriminative ability of the first version of the stroke population model was poor, indicating that it was difficult to differentiate virtual stroke patients from real stroke patients. Distributions of the virtual stroke population characteristics as well ass the correlations between the parameters were similar to what has been observed in cohorts of real stroke patients (Figure 1).
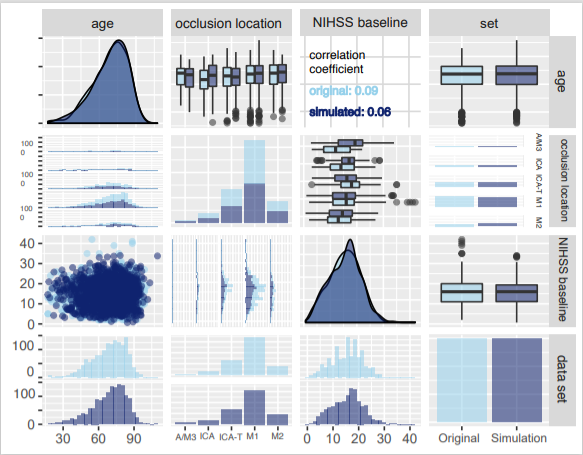
Figure 1. A selection of the distributions in the virtual stroke population versus a real stroke patient cohort
Currently, we are extending the first version of the virtual population model with three additional prognostic clinical characteristics. Anatomical features, like intracranial vessel geometries and clot histological parameters will be linked to clinical and imaging characteristics incorporated in the virtual stroke population model. The updated versions of the population model will be externally validated in the coming months.
Furthermore, we have developed an online tool from which cohorts of virtual stroke patients can be sampled based on in-and exclusion criteria of interest. This tool will be integrated within the in silico stroke trial platform (Figure 2).
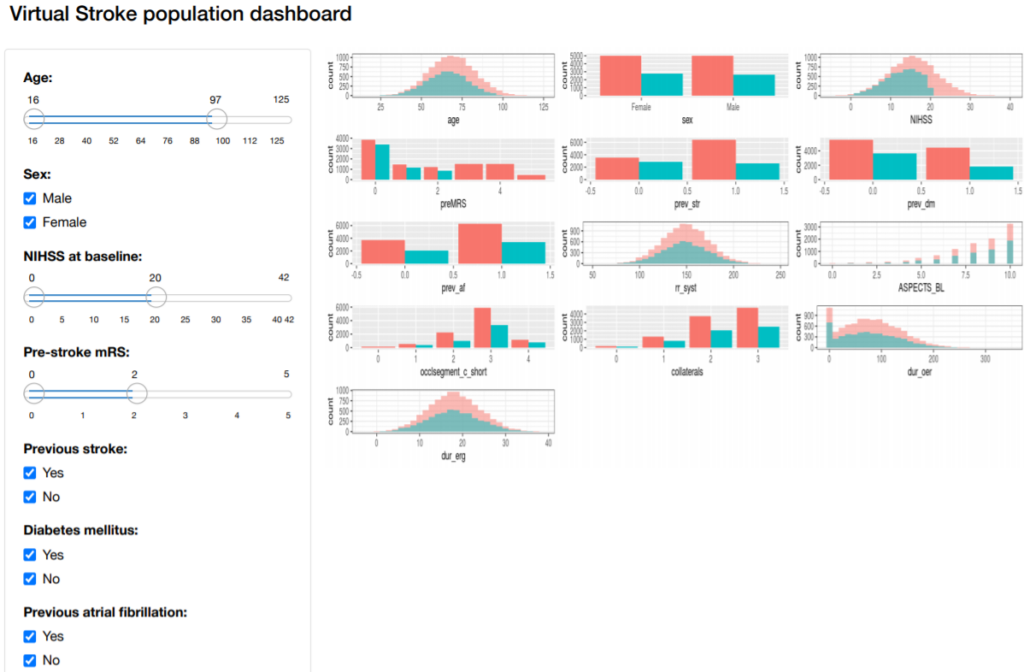
Figure 2. The virtual stroke population dashboard
Clinical outcome estimation after virtual stroke treatment
In work package 2, we are developing statistical models to estimate clinical outcome for cohorts of virtual stroke patients after virtual stroke treatment. For this estimation, the outcome of virtual treatment models (e.g. recanalization success) and tissue perfusion models (follow-up infarct volume) will be used as predictors. Besides, the virtual patient characteristics will also be included in the statistical models improve the prediction of clinical outcomes like National Institutes of Health Stroke Scale (NIHSS) and modified Rankin Score (mRS).
Imaging features of clots related to clot composition
We have created a broad analysis of clot characteristics derived from non-contrast computed tomography and CT angiography, conducted at admission of 332 ischemic stroke patients in the MR CLEAN Registry. After this, we have assessed the relationship between the imaging features of these clots to their histological composition. These findings served as input for work packages 3 and 4.
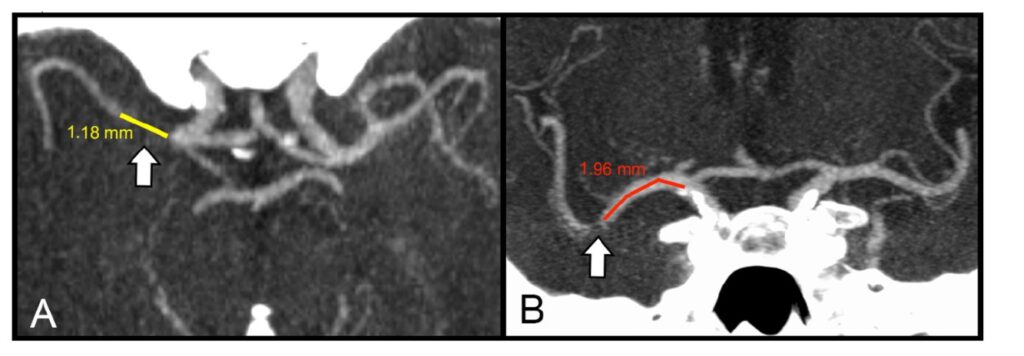
Figure 3. Measurements of clot characteristics on admission computed tomography of stroke patients. (A: clot length, B: distance from ICA-terminus to the clot).
Biomechanical thrombus analysis
From July 1st to October 3rd, we have performed biomechanical characterization and histological analysis of 41 clots from 19 acute ischemic stroke patients in the Erasmus Medical Center in Rotterdam. The results of this study are currently being prepared for scientific publication.
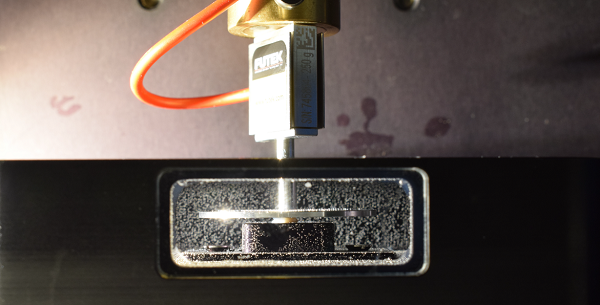
Figure 4. Close-up of the in-house developed force tester, that was used for the mechanical characterization of human stroke thrombi in Rotterdam.
Update October 2021:
Launch of virtual stroke patient cohorts As part of INSIST, we have created a public version of our virtual stroke patient model. This model is available through a web application, which enables users to generate and download dataset of virtual stroke patients according to the characteristics of interest (allowing to simulate inclusion and exclusion criteria of a study population). The web application can be accessed at the following link.
